LGBTQIA+ people get breast cancer, too. The American Cancer Society estimates that almost 2 million people newly diagnosed with cancer in 2020. Of these 2M new diagnoses, up to 216,000 individuals may also be members of the LGBTQIA+ community. While it’s difficult to estimate how many of those LGBTQIA+ folks have breast cancer, we do know that breast cancer does not discriminate.
Due to stigmas, health disparities and other barriers, it may be difficult for LGBTQIA+ people to access preventive screenings or to seek help after a diagnosis. Now is a good time to make sure you’re up to date on preventive care and aware of your specific risk factors.
Here are some questions for LGBTQIA+ folks to consider when it comes to breast cancer:
1. do lesbian, gay and bisexual people have a higher risk of breast cancer?
In short, yes. But it’s not because of any biological differences between you and straight people.
LGBTQIA+ people are more likely to experience barriers to regular screenings, stigma in healthcare settings and lack of access to health care due to socioeconomic status. Since preventive screenings can catch breast cancer before symptoms appear, people who don’t get these screenings may not be diagnosed with cancer until it has progressed.
In one 2008 survey out of the United Kingdom, 1 in 12 lesbian and bisexual women (ages 50–79) said they had been diagnosed with breast cancer, compared to 1 in 20 women overall. A 2014 study (data obtained from the California Cancer Registry) found a higher incidence of breast cancer among California counties with a higher population density of lesbian women. The National LGBT Cancer Network estimates that there are more than 1 million LGBT cancer survivors (of any type of cancer) in the United States.
2. should I come out to my healthcare providers?
Your decision to talk about your sexuality and gender identity with your healthcare team is a personal one. If you do choose to come out to your care team, it can help you feel more open in discussing how treatment may affect your relationship, sex life and future fertility. In one 2020-2021 survey, 95% of LGBTQIA+ people felt that their treatment environment was equally or more welcoming after disclosing their identity.
It may also help to seek out LGBTQIA+ friendly providers. The Human Rights Campaign maintains an online tool to help you search for inclusive healthcare facilities.
3. Where can I find LGBTQ-specific support for my breast cancer experience?
Support groups for LGBTQIA+ cancer patients, survivors and caregivers do exist! You are not alone in your journey. Here are a few options to explore:
- National LGBT Cancer Network Peer Support Groups
- Young Survival Coalition Virtual Hangout for LGBTQIA+ Survivors
- CancerCare LGBTQIA+ Support Group for Women Caregivers
- Live Through This
- Young Adult Survivors United
You can also learn more from these resources:
- National LGBT Cancer Network
- CancerCare LGBTQIA+ Program
- American Cancer Society’s LGBTQ Cancer Fact Sheet
- Living Beyond Breast Cancer: LGBTQIA+ with Breast Cancer
- Breast Cancer inFocus: Getting the Care You Need as a Lesbian, Gay or Bisexual Person
Some links will navigate you away from the Resensation® website. Links outside of resensation.com are provided as a resource to the viewer, and do not constitute an endorsement or recommendation by Axogen. Axogen accepts no responsibility for or control over the content of the linked sites.
Resensation Articles

How does mastectomy impact the nerves in the breast?
One sometimes overlooked aspect of mastectomy is its impact on nerves. Read what happens to nerves during mastectomy and explore…
Read More
What happens during implant breast reconstruction with Resensation®?
By repairing sensory nerves, Resensation® enables you to potentially regain sensation to your chest. Read how this procedure works during…
Read More
how resensation® helped Leanna feel secure in her family’s future
With Resensation®, Leanna can be there to watch her kids grow up—without losing the feeling of being whole.
Read More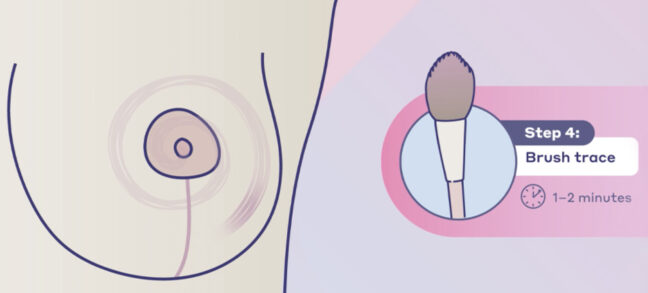
post-surgery sensory retraining: instructions and video guide
Sensory retraining is a series of exercises designed to help you reconnect with your body after breast reconstruction with Resensation®.
Read More